Abstract
Introduction:
Platelet storage pool deficiency (PSPD) is a disorder of platelet dysfunction with a varying degree of bleeding severity that can range from no symptoms to severe bleeding with hemostatic challenges. The true incidence of the disorder is unknown; however, some believe that it could be as common as von Willebrand disease (vWD). The current standard for diagnosis of PSPD is platelet electron microscopy (EM). However, there is a lack of standardization of techniques and reference ranges. In addition, some experts debate the clinical significance of the diagnosis based on the abnormal platelet EM finding alone. Available literature on adult patients with PSPD is scarce. Therefore, we conducted this study with the aim to describe the clinical and laboratory characteristics of patients diagnosed with PSPD based on specified laboratory criteria. We also intended to evaluate if platelet EM testing can be used to discern patients under evaluation for bleeding symptoms.
Methods:
We performed a retrospective cohort study of all adult patients referred for hemostatic workup who had platelet EM testing performed at The Ohio State Medical Center from 1/1/2004 to 10/26/2016. Patients with confirmed hemophilia or vWD were excluded. We collected data including patient demographics, symptoms, laboratory data, management plans, and outcomes. The reference range in our laboratory is 3.68-6.24 delta granules per platelet. Patients with less than 3.68 granules per platelet were diagnosed with PSPD (cases), while patients with at least 3.68 granules per platelet were designated as the comparison group. Characteristics in the two groups were compared by Fisher's exact test for categorical variables and the non-parametric Wilcoxon rank sum test for continuous variables since some of the continuous variables had highly skewed distributions.
Results:
A total of 291 patients were included in the study, 207 patients with PSPD based on EM results (cases) and 84 in the comparison group. Of the 207 cases, median age was 39 (range 12-84) years old and 81.2% were female. Among the cases, 38.7% had <2 delta granules per platelet, 42.0% had 2-2.99, and 19.3% had 3-3.68. The most common presenting symptom was cutaneous bruising (42.5% of cases and 38.1 % in the comparison group). Other common presenting symptoms included menorrhagia (29.9% of cases and 26.2 % of comparison), post-op bleeding (23.7% of cases and 38.1% of comparison), and epistaxis (14.0% of cases and 10.7% of comparison). At presentation, 4.8% of cases were asymptomatic. With the exception of higher incidence of post-op bleeding as a presenting symptom in the comparison group (p=0.015), there was no significant difference in the incidence of other presenting symptoms between the case and the comparison groups.
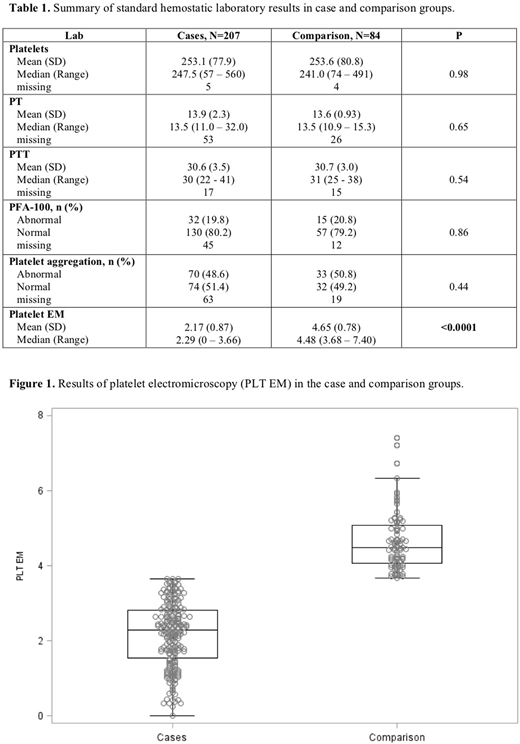
There were no significant differences in the standard hemostatic workup between the two groups, including platelet count, PT, PTT, platelet function assay (PFA-100), platelet aggregation, and von Willebrand panel (Table 1). In both case and comparison groups, 20% of patients had abnormal PFA-100 and 50% had abnormal platelet aggregation with at least one agonist. The only significant difference in the laboratory findings was platelet EM results used to categorize cases (Figure 1 and Table 1).
Conclusions:
This study showed that in adult patients referred for hemostatic workup, abnormal platelet EM does not correlate with bleeding symptoms or the results of other laboratory tests such as PFA-100 or platelet aggregation. This calls into question the relevance of abnormal platelet EM alone and the appropriate "reference range" in the adult population. Patients with delta granules below the reference range were commonly diagnosed with PSPD, and interventions such as desmopressin and/or antifibrinolytic agents were subsequently recommended. Over-diagnosis of PSPD is a concern, but under-diagnosis in patients with normal EM but persistent bleeding symptoms is also problematic. Future research is needed to characterize correlation of platelet EM values with severity of clinical presentation and to establish appropriate reference range. Furthermore, better diagnostic tools are needed to evaluate patients with bleeding symptoms.
Wang:Daiichi Sankyo: Consultancy, Other: Travel.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal